What is Eczema?
Eczema is a skin condition that causes dryness, itching, and red, inflamed rashes. It happens when the skin’s protective barrier becomes weak, making it harder to hold in moisture and defend against irritants. Leading to easily irritated and uncomfortable sensitive skin, .

Part of a larger group of conditions called dermatitis, eczema is marked by inflammation and can take different forms, such as atopic dermatitis or contact dermatitis. Managing it often involves strengthening the skin’s barrier and soothing irritation to reduce flare-ups.
What Happens When the Skin Barrier is Damaged?
The skin barrier’s job is to keep moisture in and block harmful substances. When it’s damaged, irritants and allergens can get in, and water escapes, leaving the skin dry and inflamed. In eczema, this weak barrier makes the skin more sensitive and prone to itching and irritation. Repairing the barrier helps reduce these symptoms and protect the skin from further damage.
What Are the Types of Eczema?
Eczema, a common skin condition, includes seven distinct types, each with specific symptoms and causes.
- Atopic Dermatitis: This is the most common type, leading to dry, itchy, and inflamed skin. It often begins in childhood, though it can appear at any age.
- Seborrheic Dermatitis: This type primarily affects areas with oil glands, such as the scalp, causing greasy, flaky, or itchy patches.
- Contact Dermatitis: Triggered by irritants or allergens, it results in red, inflamed, or blistered skin where exposure occurs.
- Nummular Eczema: recognized by round, coin-shaped spots on the arms, legs, or torso, which often lead to significant dryness.
- Dyshidrotic Eczema: Small, fluid-filled blisters develop on the hands and feet, frequently causing a burning sensation or cracked skin.
- Stasis Dermatitis: Poor circulation in the lower legs leads to swelling, discoloration, and skin irritation.
- Neurodermatitis: This type creates small, scaly patches of skin that become intensely itchy, often due to stress or repetitive scratching.
By understanding these types, individuals can better identify symptoms, determine triggers, and select effective treatment options.
What Causes Eczema?
Eczema develops due to a mix of internal and external factors. Internally, a weakened skin barrier struggles to retain moisture and block irritants. Germs and allergens enter the skin, triggering the immune system and causing inflammation, redness, and itching. Genetic mutations often make eczema worse by reducing the skin’s ability to protect itself.
Externally, harsh soaps, dry winter air, allergens, and rough fabrics irritate the skin and worsen symptoms. Exposure to these triggers makes sensitive skin uncomfortable and inflamed. Following a winter skincare routine with hydrating products helps protect the skin and reduce irritation.
What are Common Symptoms of Eczema?
Eczema often causes dry, itchy skin with redness, blisters, or sores. In more severe cases, the skin cracks, flakes, and becomes scaly. It typically affects the hands, feet, inner elbows, backs of the knees, and areas like the face, neck, or chest.
This condition lasts long-term and cycles between periods of improvement and worsening symptoms. Consistent skincare helps manage its effects and keep the skin healthy.
What Triggers Eczema?
Environmental factors like harsh soaps, dry air, and scratchy fabrics often trigger eczema. Sweat and allergens, including pollen and pet dander, frequently aggravate symptoms. Stress and anxiety increase skin sensitivity, making the condition worse. Certain foods also affect some people, though not everyone experiences this connection. Recognizing and avoiding triggers is crucial for effective management.
Diagnosis of Eczema
This condition is diagnosed through a physical examination of the skin. Allergy tests, blood work, or a skin biopsy may also be used to identify triggers or rule out other conditions.
Treatment Options
Treating this condition requires targeted approaches to reduce inflammation, restore the skin, and relieve symptoms:
- Reduce Inflammation: Apply corticosteroids or tacrolimus to affected areas to soothe redness, swelling, and itching.
- Repair the Skin Barrier: Use hydrating creams and emollients regularly to strengthen the skin and lock in moisture.
- Try Advanced Medications: Take immune-modulating drugs or biologics like dupilumab for severe or persistent symptoms, under medical supervision.
- Use Light Therapy: Opt for narrowband UVB treatments when other therapies don’t improve symptoms.
- Control Triggers: Avoid irritants such as allergens, harsh soaps, and synthetic fabrics to support other treatments and prevent worsening symptoms.
Managing Eczema in Children
- Moisturize Regularly: Use hydrating and barrier-repairing creams multiple times a day, especially after short, lukewarm baths.
- Treat Visible Lesions: Apply anti-inflammatory topical treatments like corticosteroids or tacrolimus to sensitive areas such as the face and neck.
- Avoid Triggers: Prevent irritation by steering clear of allergens, scratchy fabrics, and harsh soaps.
- Choose Gentle Products: Wash clothing and bedding with fragrance-free, hypoallergenic detergents.
Managing Eczema in Adults
- Follow a Consistent Routine: Apply hydrating creams and barrier-stabilizing treatments daily to reduce dryness.
- Use Proactive Treatments: Treat areas prone to relapse with tacrolimus or mid-potency corticosteroids on a long-term, intermittent basis.
- Try UV Therapy: Narrowband UVB or UVA1 treatments can address resistant symptoms.
- Address Stress: Psychosomatic counselling can reduce stress-induced exacerbations and improve overall outcomes.
- Tailor Diet Appropriately: Only follow elimination diets if food allergies are confirmed by medical testing.
- Dupilumab: It received approval from the US Food and Drug Administration(FDA) for moderate-to-severe atopic dermatitis in 2017,[7] and for asthma in 2018
- Consider Systemic Therapies: In severe cases, options like dupilumab ( It received approval from the US Food and Drug Administration(FDA) for moderate-to-severe atopic dermatitis in 2017, and for asthma in 2018) or Janus kinase inhibitors may help, but regular monitoring is necessary.
How Dupilumab Treats Severe Eczema
Dupilumab, approved by the FDA in 2017, is an effective treatment for moderate-to-severe eczema. A case study demonstrated its success in patients with severe skin involvement, including areas like the groin and folds. Before treatment, clinical images showed inflamed and damaged skin. After 6 months of therapy, significant improvement was observed, with clear signs of healing and remission.
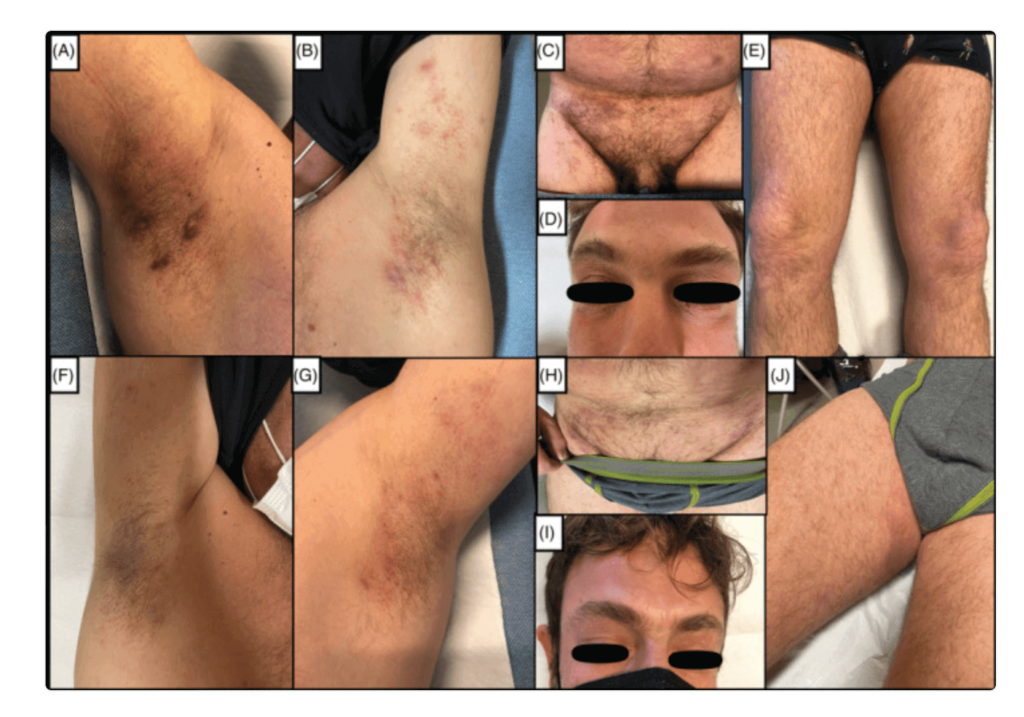
Dupilumab provides a safe and effective option for long-term eczema relief, especially in difficult-to-treat cases.
How to Prevent Eczema Symptoms
- Moisturize Daily: Use gentle, fragrance-free creams to keep the skin hydrated and protect the barrier.
- Stay Hydrated: Drink plenty of water throughout the day to support your skin from within.
- Choose Gentle Products: Use mild soaps and detergents specifically designed for sensitive skin.
- Use Proper Skincare in Winter: Switch to richer moisturizers and apply them frequently during colder months. Pair this with a humidifier to combat dry indoor air.
- Reduce Stress: Practice yoga, meditation, or other calming activities to minimize stress-related symptoms.
- Avoid Known Triggers: Identify and steer clear of irritants like allergens, harsh fabrics, and environmental pollutants.
Living with Eczema
Managing eczema requires consistency and awareness. Symptoms often come and go, with periods of calm followed by worsening skin irritation. To stay in control, follow a regular skincare routine using gentle moisturizers and mild cleansers.
Avoid known triggers, such as stress, allergens, or harsh weather conditions, to reduce irritation. Drink plenty of water to stay hydrated, and choose soft, breathable fabrics to prevent friction against sensitive skin.
With consistent care and attention to triggers, you can minimize discomfort and maintain healthier skin.
When to See a Healthcare Provider for Eczema
See a healthcare provider if eczema symptoms get worse or become hard to manage. Get medical help if your skin feels painful, inflamed, or shows signs of infection like swelling, warmth, or pus. Persistent itching that affects your sleep or daily life also needs attention.
Before your visit, prepare questions to ask. Discuss treatments, ways to avoid triggers, and if advanced therapies are an option. Knowing the right steps can help you better control eczema.
Conclusion
Managing eczema requires a combination of proper treatment, consistent skincare, and identifying triggers to keep symptoms under control. While options like moisturizers, anti-inflammatory treatments, and lifestyle adjustments help manage mild cases, advanced therapies like dupilumab offer relief for severe eczema. Seeking guidance from a healthcare provider ensures the most effective treatment plan tailored to individual needs.
By staying informed, proactive, and patient with care routines, individuals can achieve healthier skin and improve their overall quality of life.



